
Hospital bosses failed to investigate allegations against Lucy Letby and tried to silence doctors, the lead consultant at the neonatal unit where she worked has told the BBC.
The hospital also delayed calling the police despite months of warnings that the nurse may have been killing babies.
The unit’s lead consultant Dr Stephen Brearey first raised concerns about Letby in October 2015.
No action was taken and she went on to attack five more babies, killing two.
Letby has been found guilty of murdering seven babies and attempting to murder six others in a neonatal unit at the Countess of Chester Hospital, in Cheshire.
The first five murders all happened between June and October 2015 and – despite months of warnings – the final two were in June 2016.
BBC Panorama and BBC News have been investigating how Letby was able to murder and harm so many babies for so long.
We spoke to the lead consultant in the unit – who first raised concerns about Letby – and also examined hospital documents. The investigation reveals a catalogue of failures and raises serious questions about how the hospital responded to the deaths.
Dr Brearey says he demanded Letby be taken off duty in June 2016, after the final two murders. Hospital management initially refused.
The BBC investigation also found:
- The hospital’s top manager demanded the doctors write an apology to Letby and told them to stop making allegations against her
- Two consultants were ordered to attend mediation with Letby, even though they suspected she was killing babies
- When she was finally moved, Letby was assigned to the risk and patient safety office, where she had access to sensitive documents from the neonatal unit and was in close proximity to senior managers whose job it was to investigate her
- Deaths were not reported appropriately, which meant the high fatality rate could not be picked up by the wider NHS system, a manager who took over after the deaths has told the BBC
- As well as the seven murder convictions, Letby was on duty for another six baby deaths at the hospital – and the police have widened their investigation
- Two babies also died while Letby was working at Liverpool Women’s Hospital
Summer 2015: ‘Not nice Lucy’
Before June 2015, there were about two or three baby deaths a year on the neonatal unit at the Countess of Chester Hospital. But in the summer of 2015, something unusual was happening.
In June alone, three babies died within the space of two weeks. The deaths were unexpected, so Dr Stephen Brearey, the lead consultant at the neonatal unit, called a meeting with the unit manager, Eirian Powell, and the hospital’s director of nursing Alison Kelly.
“We tried to be as thorough as possible,” Dr Brearey says. A staffing analysis revealed Lucy Letby had been on duty for all three deaths. “I think I can remember saying, ‘Oh no, it can’t be Lucy. Not nice Lucy,'” he says.
The three deaths seemed to have “nothing in common”. Nobody, including Dr Brearey, suspected foul play.

But by October 2015, things had changed. Two more babies had died and Letby had been on shift for both of them.
By this point, Dr Brearey had become concerned Letby might be harming babies. He again contacted unit manager Eirian Powell, who didn’t seem to share his concerns.
In an email, from October 2015, she described the association between Letby and the unexpected baby deaths as “unfortunate”. “Each cause of death was different,” she said, and the association with Letby was just a coincidence.
Senior managers didn’t appear to be worried. In the same month – October 2015 – Dr Brearey says his concerns about Letby were relayed to director of nursing Alison Kelly. But he heard nothing back.
Dr Brearey’s fellow consultants were also worried about Letby. And it wasn’t just the unexpected deaths. Other babies were suffering non-fatal collapses, meaning they needed emergency resuscitation or help with breathing, with no apparent clinical explanation. Letby was always on duty.
In February 2016, another consultant, Dr Ravi Jayaram, says he saw Letby standing and watching when a baby – known as Baby K – seemed to have stopped breathing.
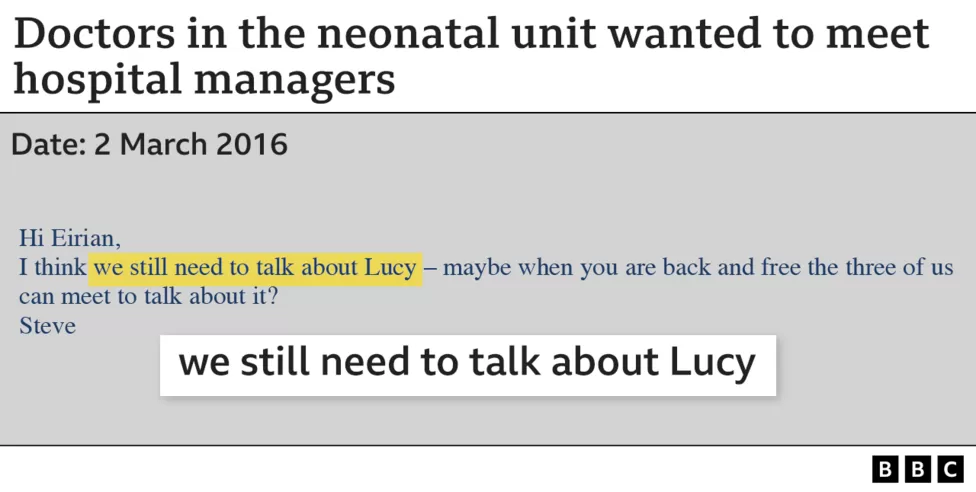
Dr Brearey contacted Alison Kelly and the hospital’s medical director Ian Harvey to request an urgent meeting. In early March, he also wrote to Eirian Powell: “We still need to talk about Lucy”.
Three months went by, and another two babies almost died, before – in May that year – Dr Brearey got the meeting with senior managers he had been asking for. “There could be no doubt about my concerns at that meeting,” he says.
But others at the meeting appeared to be in denial. Dr Brearey said Mr Harvey and Ms Kelly listened passively as he explained his concerns about Letby. But she was allowed to continue working.
June 2016: The tipping point
By early June, yet another baby had collapsed. Then, towards the end of the month, two of three premature triplets died unexpectedly within 24 hours of each other. Letby was on shift for both deaths.
After the death of the second triplet, Dr Brearey attended a meeting for traumatised staff.
He says while others seemed to be “crumbling before your eyes almost”, Letby brushed off his suggestion that she must be tired or upset. “No, I’m back on shift tomorrow,” she told him. “She was quite happy and confident to come into work,” he says.
For Dr Brearey and his fellow consultants, the deaths of the two triplets were a tipping point. That evening, Dr Brearey says he called duty executive Karen Rees and demanded Letby be taken off duty. She refused.
Dr Brearey says he challenged her about whether she was making this decision against the wishes of seven consultant paediatricians – and asked if she would take responsibility for anything that might happen to other babies the next day. He says Ms Rees replied “yes”.
The following day, another baby – known as Baby Q – almost died, again while Letby was on duty. The nurse still worked another three shifts before she was finally removed from the neonatal unit – more than a year after the first incident.
The suspicious deaths and collapses then stopped.
Letby still wasn’t suspended, however.
Instead, she was moved to the hospital’s risk and patient safety office. Here she is believed to have had access to sensitive documents relating to the hospital’s neonatal unit. She also had access to some of the senior managers whose job it was to investigate her.
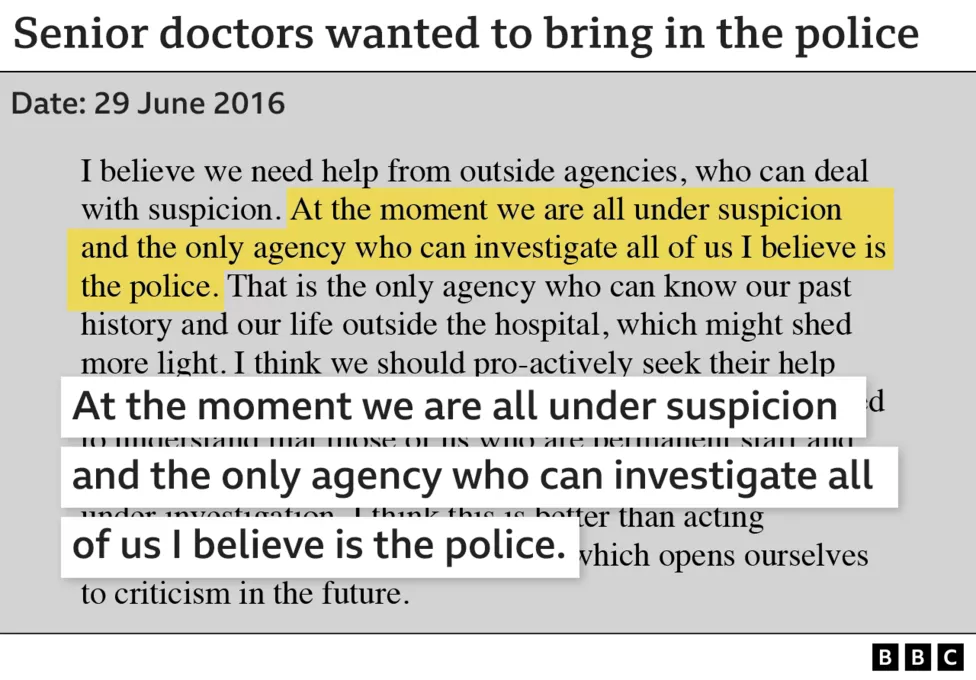
On 29 June 2016, one of the consultants sent an email under the subject line: “Should we refer ourselves to external investigation?”
“I believe we need help from outside agencies,” he wrote. “And the only agency who can investigate all of us, I believe, is the police.”
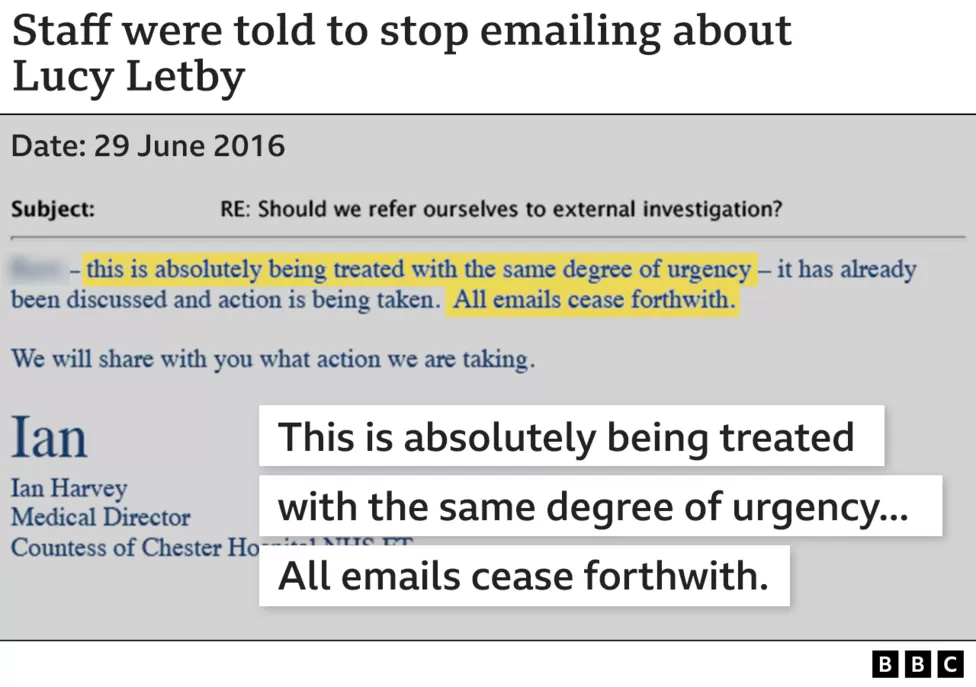
But hospital managers thought otherwise. “Action is being taken,” wrote medical director Ian Harvey in his reply. “All emails cease forthwith.”
Two days later, the consultants attended a meeting with senior management. They say the head of corporate affairs and legal services, Stephen Cross, warned that calling the police would be a catastrophe for the hospital and would turn the neonatal unit into a crime scene.
Rather than go to the police, Mr Harvey invited the Royal College of Paediatrics and Child Heath (RCPCH) to review the level of service on the neonatal unit.
In early September 2016, a team from the Royal College visited the hospital and met the paediatric consultants.
The RCPCH completed its report in November 2016. Its recommendations included: “A thorough external independent review of each unexpected neonatal death.”
In October 2016, Ian Harvey also contacted Dr Jane Hawdon, a premature baby specialist in London, and asked her to review the case notes of babies who had died on the neonatal unit.
The result was a highly caveated report. According to Dr Hawdon, her report was “intended to inform discussion and learning, and would not necessarily be upheld in a coroner’s court or court of law”.
It was not the thorough review the consultants had wanted – or the thorough external independent review that the RCPCH had recommended. But even the limited case-note report by Dr Hawdon recommended that four of the baby deaths be forensically investigated.
That did not happen.
Early 2017: Still no police inquiry
In early January 2017, the hospital board met and Mr Harvey presented the findings of the two reviews. Both had recommended further investigation of some of the baby deaths – and yet that message did not reach board members.
Records of the meeting show Mr Harvey saying the reviews concluded the problems with the neonatal unit were down to issues with leadership and timely intervention.
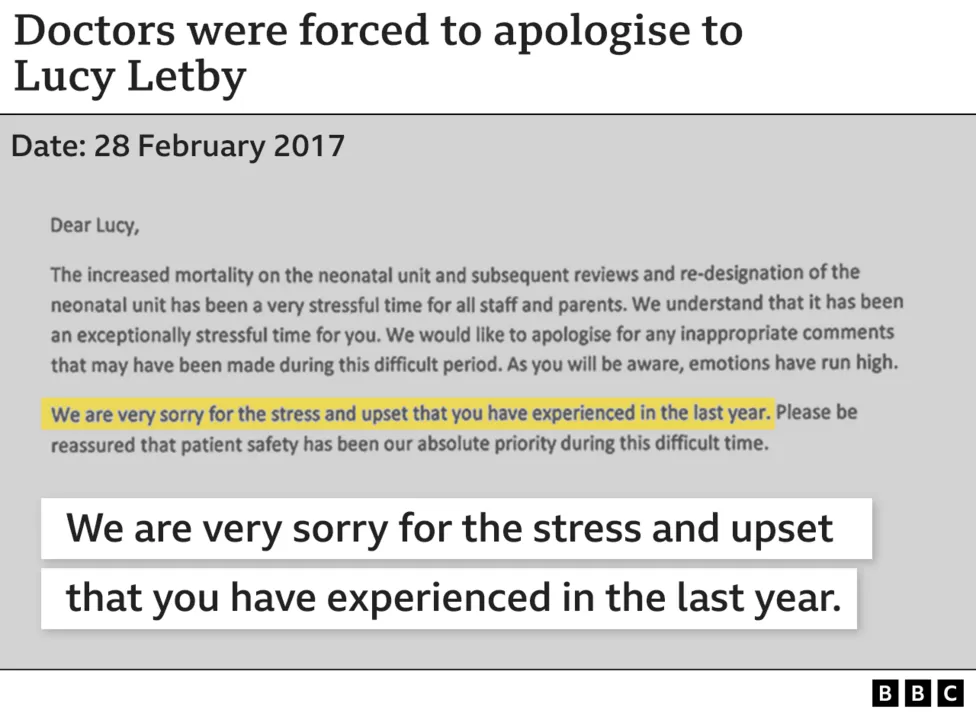
A few weeks later, in late January 2017, the seven consultants on the neonatal unit were summoned to a meeting with senior managers, including Mr Harvey and the hospital’s CEO Tony Chambers.
Dr Brearey says the CEO told them he had spent a lot of time with Letby and her father and had apologised to them, saying Letby had done nothing wrong. Mr Chambers denies saying Letby had done nothing wrong. He said he was paraphrasing her father.
According to the doctor’s account, the CEO also insisted the consultants apologise to Letby and warned them that a line had been drawn and there would be “consequences” if they crossed it.
Dr Brearey says he felt managers were trying to “engineer some sort of narrative” that would mean they did not have to go to the police. “If you want to call that a cover-up then, that’s a cover-up,” he says now.
Managers also ordered two of the consultants to attend mediation sessions with Letby, in March 2017. One of the doctors did sit down with the nurse to discuss her grievance, but Dr Brearey did not.
Yet, the consultants didn’t back down. Two months after the apology, the hospital asked the police to investigate. It was the consultants who had pushed them into it.
Dr Brearey and his colleagues finally sat down with Cheshire Police a couple of weeks later. “They were astonished,” he says.
The next day, Cheshire Police launched a criminal investigation into the suspicious baby deaths at the Countess of Chester Hospital. It was named Operation Hummingbird.
Mr Chambers told the Panorama his comments to consultants had been taken out of context and that prompt action had been taken after he was first told of serious concerns in June 2016 – including reviews of deaths.
Spring 2018: Evidence of a poisoner
Letby had not yet been arrested and was still working at the hospital’s risk and patient safety office. But Operation Hummingbird was in full swing and Dr Brearey was helping the police with their investigation.
Late one evening, he was going through some historic medical records when he discovered a blood test from 2015 for one of the babies on his unit. It recorded dangerous levels of insulin in the baby’s bloodstream.
The significance of the test result had been missed at the time.
The body produces insulin naturally, but when it does, it also produces a substance called C-Peptide. The problem with the insulin reading that Dr Brearey was looking at was that the C-Peptide measurement was almost zero. It was evidence the insulin had not been produced naturally by the baby’s body and had instead been administered.
“It made me feel sick,” Dr Brearey recalls. “It was quite clear that this baby had been poisoned by insulin.”

A few months later, Letby was finally arrested and suspended by the hospital. But three years had passed since Dr Brearey had first sounded the alarm.
When a new medical director and deputy chief executive, Dr Susan Gilby, began work the month after Letby’s arrest, she was shocked at what she found.
She says her predecessor, Mr Harvey, had warned her she would need to pursue action with the General Medical Council, the doctor’s regulator, against the neonatal unit’s consultants – those who had raised the alarm. Mr Harvey denies this.
However, inside a box of files left in his office, Dr Gilby found evidence the problems lay elsewhere. Marked with the word “neonates”, the files revealed how a meeting of the executive team in 2015 had agreed to have the first three deaths examined by an external organisation. That never happened.
The management team had also failed to report the deaths appropriately. It meant the wider NHS system could not spot the high fatality rates. The board of the hospital trust was also unaware of the deaths until July 2016.
Dr Gilby says the trust’s refusal to call police appeared to be heavily influenced by how it would look. “Protecting their reputation was a big factor in how people responded to the concerns raised,” she says.
Later in 2018, after Tony Chambers resigned, Dr Gilby was appointed chief executive and she stayed in post until 2022. She is now suing the trust for unfair dismissal.
Dr Brearey, says hospital managers had been “secretive” and “judgemental” throughout the period leading up to the nurse’s arrest.
“There was no credibility given to our opinions. And from January 2017, it was intimidating, and bullying to a certain extent,” he tells BBC News. “It just all struck me as the opposite of a hospital you’d expect to be working in, where there’s a safe culture and people feel confident in speaking out.”
Letby would ultimately be charged with seven murders and 15 attempted murders between June 2015 and June 2016. She was found guilty of all seven murders and seven attempted murders.
She was found not guilty of two counts of attempted murder. The jury also failed to reach a verdict on a further six counts of attempted murder, including all charges related to Baby K and Baby Q.
In a statement, Tony Chambers, the former CEO, said: “All my thoughts are with the children at the heart of this case and their families and loved ones at this incredibly difficult time. I am truly sorry for what all the families have gone through.
“The crimes that have been committed are appalling and I am deeply saddened by what has come to light. As chief executive, my focus was on the safety of the baby unit and the wellbeing of patients and staff. I was open and inclusive as I responded to information and guidance.”
He added: “I will co-operate fully and openly with any post-trial inquiry.”
Ian Harvey said in a statement: “At this time, my thoughts are with the babies whose treatment has been the focus of the trial and with their parents and relatives who have been through something unimaginable and I am sorry for all their suffering.
“As medical director, I was determined to keep the baby unit safe and support our staff. I wanted the reviews and investigations carried out, so that we could tell the parents what had happened to their children. I believe there should be an inquiry that looks at all events leading up to this trial and I will help it in whatever way I can.”
The Countess of Chester Hospital is now under new management and the neonatal unit no longer looks after such sick babies.
The current medical director at the hospital, Dr Nigel Scawn, said the whole trust was “deeply saddened and appalled” by Letby’s crimes.
He said “significant changes” had been made at the hospital since Letby worked there and he wanted to “provide reassurance to every patient who accesses our services that they can have confidence in the care that they will receive”.
Since Letby left the hospital’s neonatal unit, there has been only one death in seven years.






























